Can Cannabis Help with Cancer?

Medical research continues to show the therapeutic benefits of cannabis. Studies have found that inhaled cannabis (smoked or vaped) could help treat neuropathic pain caused by damaged nerves or improve food intake in HIV patients. In the context of cancer, several small studies have long suggested that smoked or vaporized cannabis can help with nausea and vomiting caused by chemotherapy.
While cannabis remains a powerful tool for cancer symptom management, new large-scale analyses and clinical guidelines are refining how we understand its role in oncology. Researchers are increasingly focused on where cannabinoids show the most reliable benefits—such as pain, nausea, and appetite support—while also clarifying limitations, dosing considerations, and patient safety. This evolving evidence is helping move cannabis toward more standardized, evidence-based care.
The ‘Anti-Tumor’ Debate: What the Latest Science Says
While earlier reports focused on petri dish and animal studies showing that THC and CBD slowed the growth of certain cancer cells (apoptosis), 2025 has brought more comprehensive data to the table.
The largest-ever meta-analysis on the subject, published in Frontiers in Oncology (2025), reviewed over 10,000 studies. It found overwhelming scientific support for cannabis’s potential to treat symptoms, but it also pointed to a growing consensus on its potential “anti-cancer” activity. Specifically:
- Synergistic Effects: Latest research into ovarian cancer cells suggests that a 1:1 THC:CBD ratio may be more effective at inhibiting cancer cell migration and spreading than either compound alone.
- Survival Rates: A pilot trial involving 21 patients showed that those receiving cannabis-based medication alongside traditional chemotherapy survived longer than the placebo group.
- Cautionary Findings: Conversely, a 2024 study suggested that “cannabis use disorder” might be linked to higher risks of certain head and neck cancers, though experts argue this may be due to confounding factors like tobacco use.
Standard Cannabis-Based Drugs in Oncology
Several pharmacological drugs derived from cannabis or synthetic cannabinoids are currently integrated into cancer care:
- Dronabinol (Marinol, Syndros): An FDA-approved THC-based medicine for chemotherapy-induced nausea and vomiting (CINV).
- Nabilone (Cesamet): A synthetic cannabinoid that mimics THC, prescribed when standard anti-nausea drugs fail.
- Nabiximols (Sativex): A 1:1 THC:CBD mouth spray. While widely used in Europe and Canada for cancer pain and MS spasms, it is still undergoing clinical review in the US as of late 2025.
Development of New Cannabis Drugs: A first-of-its-kind phase 2/3 clinical trial found that oral THC:CBD cannabis capsules improved complete response rates for chemotherapy-induced nausea and vomiting, but also caused significantly more side effects. Despite being hailed as an important step forward, experts say limitations in design and unresolved challenges in cannabis research mean the findings aren’t yet broadly applicable and further study is needed.
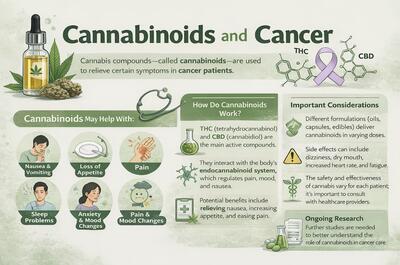
How Cannabis Affects Symptoms and Treatment
While cannabinoid drugs are not a “cure,” they can offer vital relief for several symptoms. However, the 2024 ASCO Guidelines issued a crucial update: clinicians now recommend against using cannabis as a direct cancer treatment unless it is part of a clinical trial.
Instead, cannabis is viewed as an adjunctive therapy. It is most effective for:
- Refractory Nausea: When standard-of-care medicines don’t work.
- Chronic Pain: Particularly nerve pain where opioids may be ineffective or unwanted.
- Sleep and Mood: Recent surveys from NCI-designated centers show that 20-50% of cancer patients use cannabis, primarily citing better sleep and reduced anxiety as the top benefits.
Side Effects and Safety Considerations
Cannabis is not without risks. Patients frequently report drowsiness, dizziness, and dry mouth. More critically:
- Immunotherapy Interactions: Some studies suggest cannabis might interfere with the effectiveness of certain immunotherapies (checkpoint inhibitors), making it vital to discuss use with an oncologist.
- Mental Health: Synthetic cannabinoids like Nabilone can occasionally trigger hallucinations or worsen depression in predisposed individuals.
- Purity: Patients are urged to use lab-tested medical products to avoid contaminants like mold or heavy metals, which can be dangerous for immunocompromised patients.
FAQ: Cannabis, Cancer, and Health
1. Can cannabis cure cancer? Current scientific consensus (including the most recent updates from the American Cancer Society) states that cannabis does not cure cancer. While lab studies show it can kill cancer cells in test tubes, large-scale human clinical trials have not yet proven it can reliably cure or even stop the disease in humans.
2. Should I stop chemotherapy to use cannabis oil? No. Relying on cannabis alone while avoiding conventional treatment can have life-threatening consequences. Cannabis should be used as a supportive therapy alongside standard medical care.
3. Is CBD or THC better for cancer patients? Most recent research suggests a 1:1 ratio of THC to CBD provides the most balanced benefit for pain and nausea. THC is primarily responsible for appetite stimulation and nausea relief, while CBD helps modulate pain and may reduce the “high” or anxiety caused by THC.
4. Can I use cannabis if I am on immunotherapy? You must consult your doctor. There is emerging evidence that cannabinoids might suppress the immune response required for certain immunotherapies to work effectively.
5. Is smoking cannabis safe for cancer patients? Inhaling smoke contains many of the same carcinogens as tobacco. For patients with weakened immune systems or lung-related cancers, doctors generally prefer edibles, sublingual oils (under the tongue), or vaporizers over smoking.
6. Does cannabis help with ‘Chemo Brain’? While some patients report that cannabis helps with the stress of “chemo brain,” others find it can worsen short-term memory and concentration. Its effect on cognitive function varies greatly by dosage and individual.
7. What types of cannabis-based drugs are used in cancer treatment? Several pharmacological drugs derived from cannabis are already used to support cancer patients, either during active treatment or in later stages of the disease. These medications are primarily prescribed to manage symptoms such as nausea, vomiting, pain, and appetite loss.
8. What is Dronabinol and how is it used? Dronabinol (sold under the brand names Marinol and Syndros) is a THC-based medication approved by the U.S. Food and Drug Administration (FDA). It is commonly prescribed to treat nausea and vomiting caused by cancer chemotherapy and to help stimulate appetite and prevent weight loss, particularly in patients with AIDS.
9. What is Nabilone? Nabilone (Cesamet) is a synthetic cannabinoid that mimics the effects of THC. It is prescribed to cancer patients experiencing severe nausea and vomiting from chemotherapy, especially when standard anti-nausea medications are ineffective. Nabilone is also FDA-approved for use in the United States.
10. What is Nabiximols and where is it available? Nabiximols is an oral spray containing a balanced formulation of THC and CBD. It is used to manage cancer-related pain, as well as muscle spasms and pain associated with multiple sclerosis (MS). While nabiximols is available in Canada and several European countries, it has not yet been approved for use in the United States.
11. Why is regular cancer screening important, even if you feel healthy? Many cancers can develop without noticeable symptoms in their early stages. Regular screenings (such as mammograms, colonoscopies, skin checks, or prostate exams) can help detect cancer earlier, when treatment options are often more effective and outcomes are generally better.
12. How do lifestyle habits like smoking affect cancer risk and monitoring? Smoking is a well-established risk factor for several types of cancer, particularly lung, throat, and oral cancers. People who smoke or have a history of smoking may benefit from more frequent health checkups and discussions with healthcare providers about lung health and cancer risk. Paying attention to persistent symptoms—such as chronic coughing, shortness of breath, or unexplained fatigue—and seeking medical advice early can make a meaningful difference.
Medical Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with your oncologist or a qualified healthcare professional before integrating cannabis into your treatment plan, especially to check for potential drug interactions.
More from Soft Secrets: